- Home
- Lab Supplies
- Microbiology Molecular Biology Supplies
.....Read More

Automated Microplate Sealers

Cell Lifters, Spreaders & Inoculating Picks

Colony Counters

Dip Slides

Electrophoresis Supplies

Hemacytometers

Histology Products
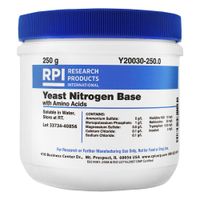
Microbiology Media

Microbiology & Staining Supplies

Paraffin Wax Dispensers & Trimmers

Petri Dishes & Well Plates

Thermal Cyclers & Blocks

Tissue Grinders
Frequently Asked Questions
What are the essential microbiology lab supplies?
How do you choose the right molecular biology reagents?
What safety equipment is necessary for handling biological samples?
How do you properly store microbiology media and reagents?
What are the best practices for culturing bacteria in a lab?
How do you ensure accuracy in DNA replication experiments?
What equipment is needed for cell culture in research facilities?
How do you dispose of biological waste safely?
What are the common challenges in using protease inhibitors?
How do you measure radioactive isotopes in biological samples?